Female fertility part one: why I chose embryo freezing at 30
Everything we know about how female fertility works & my personal experience.
This is part one of a two-part series on female fertility where I will share the most up to date information on female fertility broken down as follows:
Part one: how female fertility works, why it declines with age and my experience with embryo freezing
Part two: how to improve fertility and the future of fertility
Intro
Many years ago, I had just moved to New York and was having lunch with a woman who told me that all she ever wanted was to be a mother. “Since I was a little girl, I just wanted to find a man to marry so I could have children,” she said while cutting perfect, tiny bites into her steak. She now had the husband, three kids, and an au pair, and they all lived happily in a chic brownstone. As I walked back to my apartment (not a chic brownstone), I thought about what I had wanted since I was a little girl. The list was long, but it did not include children.
When you’re in your 20s and say that you don’t want children, most people tell you to just give it time, as it all changes once you’re older. In my case, however, even as I walked into the fertility clinic on the eve of my 31st birthday, that desire had failed to materialize. Was I completely lacking the maternal instinct? Was it because I had been blessed with a wonderful family and an amazing relationship, and there was no “void” to be filled? I couldn’t find an answer, but what I did know was that holding my beliefs at a particular point in time as forever true is not very smart.
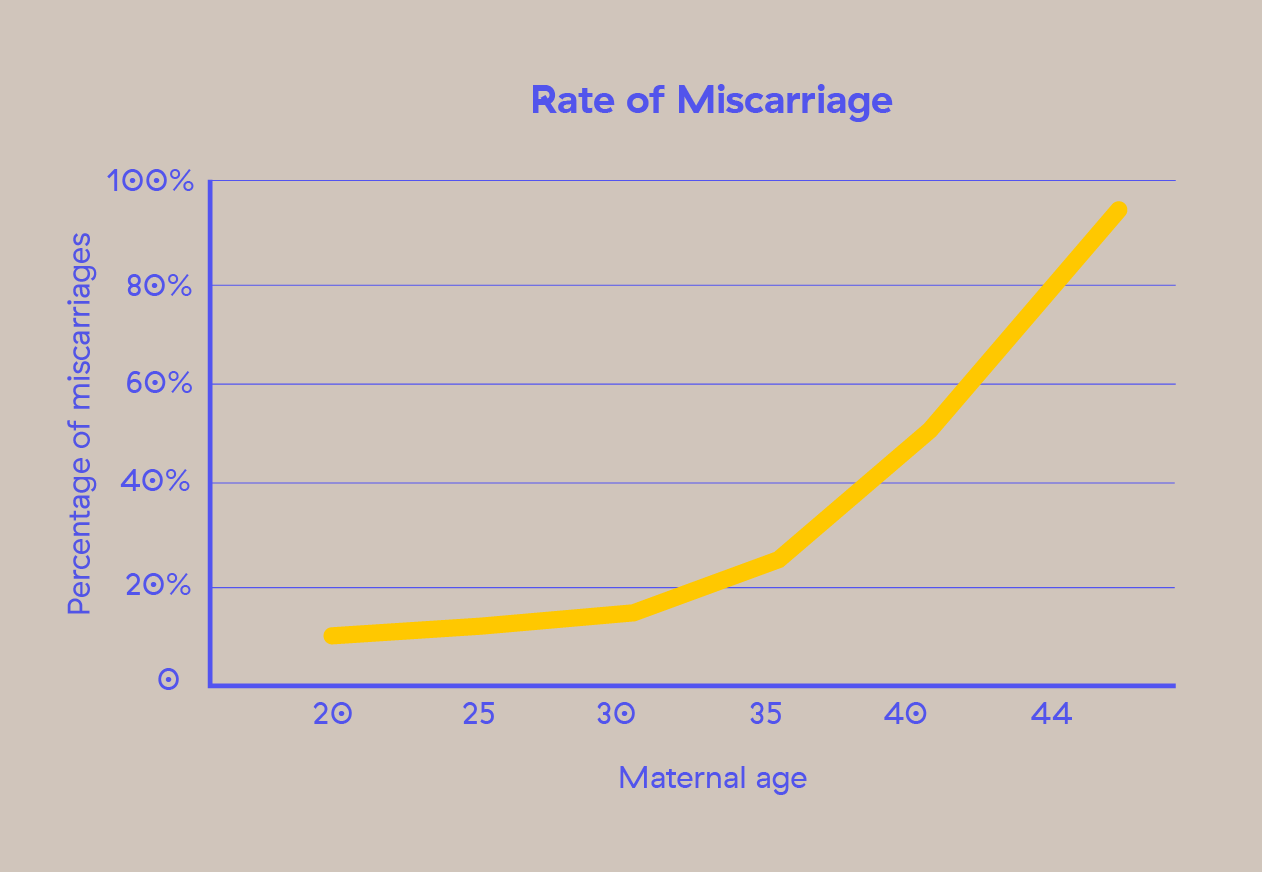
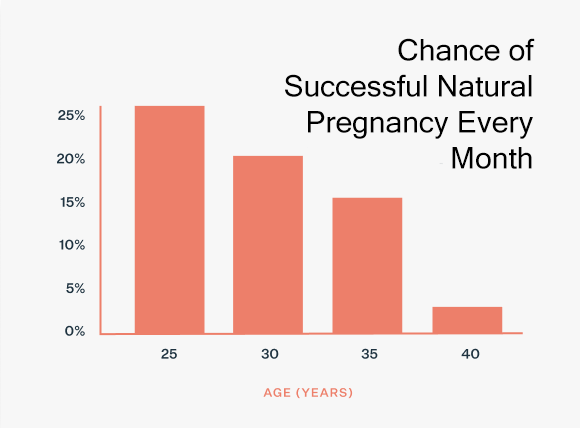
And if, say, at 37, I’d change my mind, while there is still a chance of conceiving naturally, the odds are significantly reduced to under 15% per cycle and around 50% within a year. Here’s why.
Why fertility decreases with age
1. Egg loss
As women, we are born with all the eggs we will ever have, which is approximately 1-2 million. By puberty, this number decreases to between 300,000 and 500,000 eggs. At 30, we’re left with around 120,000 eggs. Fertility starts to decline, and the rate accelerates after age 35. By age 37, the number of eggs left in the ovaries is around 25,000. By 51, the average age of menopause in the U.S., women have fewer than 1,000 eggs left in their ovaries.
The number of eggs released each month does not change with age. During each menstrual cycle, a cohort of 10-20 eggs is activated to mature, but only one egg is released during ovulation - the most mature and healthy egg in the cohort. The remaining eggs in the cohort die through a process called apoptosis, a natural cell death mechanism. This means that many eggs are lost each month, even if only one is ovulated.
2. Egg quality
But alongside ovarian reserve and egg loss, there’s another important reason why age is such a strong determinant in female fertility and that is egg quality. Imagine you have a vault inside your ovary that holds all your eggs. Every month you have a group of eggs that you are losing from the vault and from that group, one is chosen to ovulate and the rest die. As you age, the eggs that have been stored in your ovaries throughout your life accumulate the effects of wear and tear, including exposure to inflammation, toxins, and other environmental factors. This accumulation can make it more challenging for the body to select a healthy egg for ovulation. Even if pregnancy occurs, at age 37, for example, around 45% of a woman's eggs will have chromosomal abnormalities, increasing the risk of miscarriage and birth defects.
This process happens assuming a healthy lifestyle, but egg quality can be even further decreased by smoking, alcohol consumption, obesity, endometriosis, diabetes, PCOS, autoimmune conditions or cancer treatments.
3. Fecundability
Fecundability is the probability of achieving a clinically recognized pregnancy during a single menstrual cycle or month. Good egg and sperm quality significantly increase the probability of pregnancy. But even under optimal conditions, the maximum chance of a clinically recognized pregnancy is 30-40% per cycle. For healthy young couples, the probability of pregnancy per cycle is about 20-25%, with cumulative probabilities of 60% within six months, 84% within a year, and 92% within two years.
Ovulatory disorders (PCOS, thyroid dysfunction), fallopian tube issues, endometriosis, uterine fibroids, polyps, autoimmune disorders, and cancer treatments like chemotherapy can impact ovulation, implantation, and pregnancy outcomes.
Enter egg freezing
So I was almost 31 years old, Emi was 35, and neither of us was ready for kids or sure that we ever wanted them. But we both like optionality and we like to hedge our bets. We decided that the best bet would be egg freezing. As it turns out, if you are not ready to conceive by the age of 32-33, this is a good time to freeze your eggs as you you still typically have a good quantity and quality of eggs.
The reason why egg freezing is such a great hedge if you are not ready to start a family is egg quality. As outlined earlier, your eggs at age 30 are healthier than your eggs at age 35, so eggs frozen at a younger age are likely to be of higher quality, reducing the risk of chromosomal abnormalities and increasing the likelihood of a healthy pregnancy.
In terms of the psychological burden, egg freezing also gives you more control over reproductive timing. If you are pursuing other personal or professional goals, if you have not yet found the right partner, or suffer from medical conditions that impact fertility, freezing your eggs allows you to preserve your younger, healthier eggs for future use, potentially increasing the chances of a successful pregnancy later in life.
The egg freezing procedure involves stimulating the ovaries with hormonal medications to produce multiple eggs, which are then retrieved through a minor surgical procedure. The mature eggs are rapidly frozen using a method called vitrification, which prevents ice crystal formation and preserves the eggs' viability. These frozen eggs can be stored for many years and later thawed, fertilized, and implanted in the uterus when the woman is ready to conceive.
It’s important to note that egg freezing does not affect your ovarian reserve or future fertility. The process of egg freezing involves retrieving and preserving eggs that would otherwise die, so it does not reduce the overall number of available eggs in your body.
The process
1. Fertility assessment
I chose Kindbody because I have a bias toward trusting technology companies who disrupt DTC healthcare more than traditional providers. At my first appointment, we discussed our goals, medical history and I received a full overview of the egg freezing process. Then I had extensive bloodwork done to assess my general health, hormone health and fertility.
One of the tests used to get an estimation of a woman’s ovarian reserve is the Anti-Müllerian Hormone (AMH) blood test. AMH is a hormone produced by ovarian follicles (the small sacs in the ovaries that contain immature eggs). AMH levels give an indication of the number of remaining eggs with higher AMH levels generally suggesting a higher number of remaining eggs, while lower levels suggest a reduced ovarian reserve. AMH levels typically decline with age, reflecting the natural decrease in the number of eggs as a woman ages.
The American College of Obstetricians and Gynecologists does not recommend testing AMH unless you are experiencing infertility because AMH levels alone cannot predict an individual's ability to get pregnant naturally. However, if you want to make informed decisions about when to start a family, testing AMH can provide valuable insight—though not a complete picture—of your ovarian reserve. Higher AMH values are associated with better outcomes when undergoing fertility treatments like egg freezing and IVF by indicating a larger remaining egg supply that can be stimulated.
To get an even better estimate of your ovarian reserve, AMH is paired with an Antral follicle count (AFC). The AFC is determined through a transvaginal ultrasound, which allows the doctor to visualize and count the number of antral follicles present in the ovaries. The number of antral follicles is considered an indicator of a woman's ovarian reserve. A higher count suggests a greater number of remaining eggs, while a lower count suggests a reduced ovarian reserve.
Women with low AMH levels can still conceive naturally. While the chances may be lower compared to those with higher AMH levels, natural conception is still possible, especially if other fertility factors (such as regular ovulation, good egg quality, and a healthy reproductive system) are in place. But this is why testing AMH is so important if you are not ready to conceive. Imagine being 27 years old and finding out that you have a low ovarian reserve. Does that mean you can’t conceive naturally? No. But having this information can help you make important decisions about when to start trying, or deciding to freeze your eggs for future use.
If you have any medical conditions or a history of infections (including sexually transmitted infections), your doctor will also perform a tubal evaluation and pelvic ultrasound to evaluate the patency (openness) of the fallopian tubes and the structure of the reproductive organs. If you are going through this process together with a partner, you should also have a full semen analysis done to assess male fertility by evaluating sperm count, motility, morphology, and other semen parameters.
2. Deciding between egg freezing and embryo freezing
Because I knew that if I wanted children, I’d only want to have them with Emi, we decided to do embryo freezing. The key difference between egg freezing and embryo freezing lies in when fertilization occurs. With egg freezing, a woman's unfertilized eggs are extracted and frozen for potential future use. When she is ready to attempt pregnancy, the frozen eggs are thawed and fertilized with sperm to create embryos. In contrast, with embryo freezing, the eggs are fertilized with sperm immediately after retrieval through IVF, and the resulting embryos are frozen.
Here are some important considerations when choosing between the two:
The survival rate for thawed eggs varies but generally ranges between 75-90%. Embryos have higher thaw survival rates, typically between 90-95%. This higher rate is due to the fact that embryos, particularly those that have reached the blastocyst stage (5-6 days after fertilization), are more robust and less sensitive to the freezing and thawing process compared to unfertilized eggs.
Live birth rates from eggs are lower, with an estimated 2-12% chance per thawed and fertilized egg. Live birth rates from embryos are higher, with an estimated 30-50% chance per embryo transfer cycle.
With egg freezing, based on the number of eggs retrieved and your age, you can approximate the number of live births you can expect, but you can’t know how many of those eggs will actually fertilize. Embryo freezing provides more information upfront about the viability of the eggs since only the successfully fertilized eggs that develop into embryos are frozen. With frozen embryos, you know exactly what you’re getting.
Egg freezing is a better choice if you don’t have a partner because with embryo freezing, the sperm source is locked in and you can’t change your mind later on.
Egg freezing is cheaper than embryo freezing which requires paying for the full IVF process first. However, based on many eggs you are able to retrieve in one cycle and based on how many children you want, you may need more than one egg freezing cycle.
Survival, fertilization and implantation are all influenced by the quality of the eggs or embryos, the freezing technology used and the woman’s age. Even so, neither process guarantees pregnancy or live birth. Not every egg will fertilize with sperm, develop into an embryo, be genetically normal, or implant successfully, even if it is genetically normal. For instance, if you have 20 eggs, and 18 survive the freeze-thaw process, 14 fertilize, and 7 make it to the blastocyst stage, about 60-70% of these 7 embryos will be genetically normal if you are age 30. This means approximately 4 of the 7 embryos will be genetically normal. At transfer, there is at best a 65% chance of live birth per embryo. This highlights the importance of freezing eggs or embryos when egg quality is high and why you need to understand this process in detail and set realistic expectations.
3. The treatment
Eggs freezing and IVF are the same in terms of process except for what happens on the lab end when the eggs come out of your body. In egg freezing, the eggs are cryopreserved immediately after retrieval, while in IVF, the eggs are fertilized with sperm in the lab before being frozen or transferred to the uterus.
IVF involves stimulating the growth of multiple eggs that are already present in the ovaries, rather than stimulating the hyper-release of eggs. During an IVF cycle, women are given hormone medications to stimulate the growth of multiple eggs within the ovaries. This process typically lasts for 9-12 days.
The medications (gonadotropins like Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH)) stimulate the growth of multiple follicles, each containing an egg. These eggs mature simultaneously, allowing for the retrieval of multiple eggs during the egg retrieval procedure. To prevent premature ovulation, GnRH agonists or antagonists are used, ensuring eggs reach optimal maturity. About 36 hours before egg retrieval, a trigger shot of human chorionic gonadotropin (hCG) is administered to finalize egg maturation.
In my case, the IVF cycle lasted ten days, during which I did 2-3 at-home injections per day and had a blood draw and ultrasound at Kindbody every other day. I felt good throughout and only started to experience bloating and a feeling of heaviness toward the end when my eggs were ready to be retrieved. This is very common since your ovaries are normally the size of a plum, but enlarge to the size of a grapefruit by the time you’re ready for the retrieval. Kindbody has a very user-friendly interface where you get all the information you need every step of the way. There’s also a nurse available 24/7 to chat with during the process, helping you with questions, figure out the injections, and the trigger shot.
The egg retrieval procedure took about 15 minutes and I was under general anesthesia. For embryo freezing, the fresh semen sample must also be provided the day of the egg retrieval. When I woke up, my doctor told me they had retrieved 20 eggs and that I would receive the results of fertilization and embryo development in about two weeks. Of the 20 eggs, 13 were mature (only mature eggs can be fertilized) and of the 13, 8 showed signs of normal fertilization. Because we had chosen full genetic testing of embryos, of the 8 embryos we ended up with 3 chromosomally normal ones that were frozen.
I had heard from many women that IVF medication made them feel horrible both physically and mentally. While I didn’t experience much discomfort during the treatment, post egg retrieval things got more unpleasant. I had a lot of bloating and water retention that didn’t go away for weeks, cystic acne, mood swings, and irritability. It felt like PMS on steroids that lasted for about a month. I did gain a few pounds of mostly water weight and inflammation that went away once my hormones stabilized. It wasn’t great, but on a scale of 1-10 in terms of discomfort, I’d rate the entire process a 6.
Should you do egg freezing?
This is an incredibly personal choice and while egg freezing is expensive and perhaps not for everyone, here’s why I think you should consider it.
At age 25, when you walk into your ob-gyn's office, they’re not likely to bring up egg freezing because you’re still so young that you might just get pregnant on your own. However, if you’re not planning on getting pregnant anytime soon and want to be proactive, it makes sense to start thinking about freezing your eggs as early as possible to get the best outcome, meaning the highest quality eggs you can possibly get.
There are many reasons why your reproductive plans can be delayed: you want to focus on your career or other life goals, including financial stability. You don’t meet the right partner, or you do meet the right partner but other non-age-related fertility issues arise (sperm quality, fallopian tube problems PCOS, endometriosis, etc.). Or, you’re ready to have a child at age 30, but you want four kids in the future, so it’s still a good idea to freeze some eggs as a backup plan for when you’re 38.
Egg freezing offers no guarantees and isn’t really an “insurance policy,” but it gives you a higher than 0% chance of having a child and can prevent the pain and suffering that come from being without options. If you can’t grasp the emotional cost because you’re ambivalent about having children, consider the physical and financial cost of going through multiple rounds of IVF later on, which will inevitably be higher.
For me, embryo freezing was the best choice I could make and I felt so much more at ease knowing that I had created optionality for myself and my partner. The only regret I have is not doing multiple cycles. For women under 35 at the time of egg retrieval, the chances of a live birth per frozen embryo transfer are generally around 40-50%. So with three frozen embryos, that gives me a realistic chance of a 1.5 live births at best.
If you are planning on egg freezing, it is even more important to consider multiple rounds. At the time of freezing, you are preserving single-cell eggs, and you cannot determine the quality of each egg. This means you won't know how many eggs will survive the freezing and thawing process, how many will fertilize, and how many will result in a pregnancy.
In terms of cost, it varies greatly depending on your location, so listing estimates isn't very useful. Kindbody offers full transparency regarding costs, and you can get an idea by looking at their pricing. Always check with your insurance and employer as you might be able get partial or even full coverage in some cases.
I had a really positive experience with Kindbody, but you must do your own research and find a clinic that has really good outcome data with their frozen eggs, meaning enough people have come back to use their eggs and turn them into embryos and get pregnant with those embryos. If a clinic or lab discourages you from doing genetic testing on your embryos, or they don’t grow embryos past day three (cleavage stage embryos), run and don’t look back. A good clinic should be transparent about their success rates, procedures, and how up-to-date their treatments and technology are.
Next week, I will return with part two of this series, which will include a protocol for improving fertility and insights into the future of female fertility, covering both new technology and global trends. In the meantime, if you have any questions about the egg freezing process, drop me a line, and I’ll be happy to help.