Obesity epidemic part one: why half the world is overweight
Why we're fatter than ever, why we struggle to lose weight, and our current solutions.
This is part one of a two-part series on the obesity epidemic where I will share the most up to date information on obesity and overweight broken down as follows:
Part one: the context behind this unprecedented rise in obesity and the current gold-standard treatments
Part two: obesity prevention with a focus on child obesity
Intro
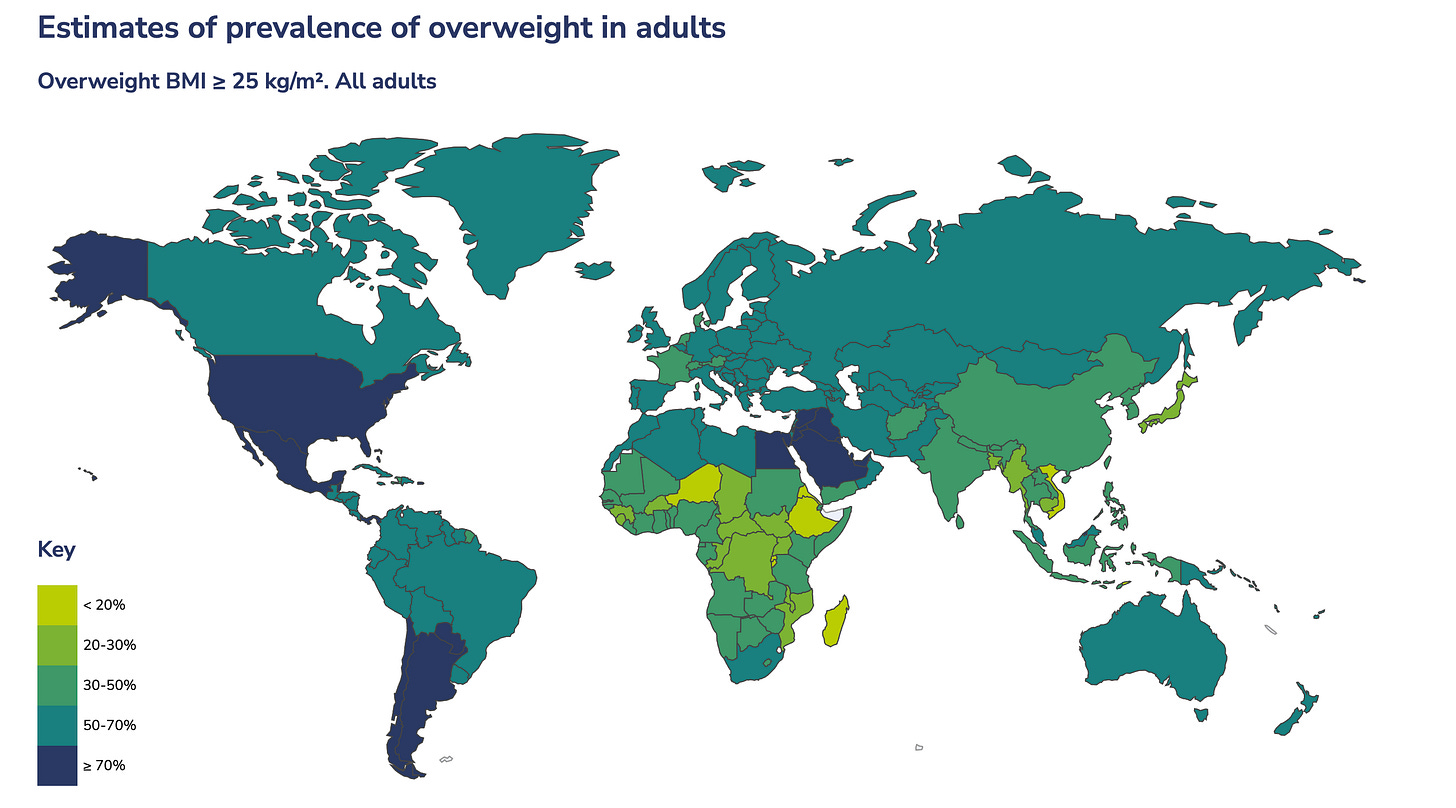
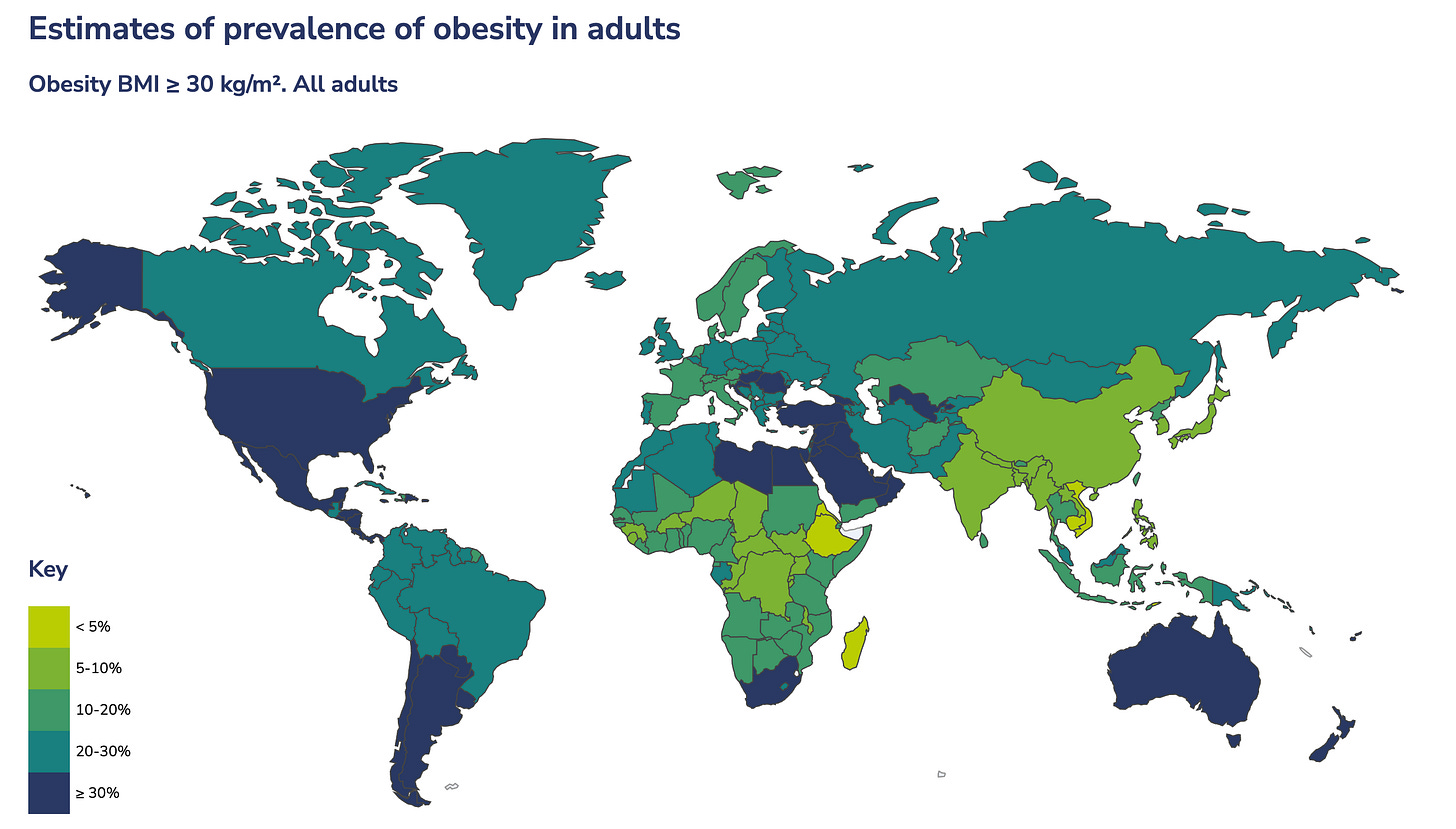
Nearly half of the world’s population is currently overweight - 43% of adults and 16% of children. Of those, over 1 billion have obesity. Obesity among adults has more than doubled since 1990, and has quadrupled among children and adolescents (5 to 19 years of age). The World Obesity Federation's 2024 World Obesity Atlas projects that the number of adults living with obesity will continue to rise, reaching 1.53 billion by 2035.
There are two reasons why obesity represents one of the biggest health crises we’ve ever experienced: it directly contributes to nearly all leading causes of death and its economic impact is projected to reach $4.32 trillion annually by 2035, which is nearly 3% of the global gross domestic product (GDP).
The US has experienced one of the most significant surges in obesity, with rates tripling over the past 60 years. However, this issue has now become a global epidemic, with low- and middle-income countries witnessing some of the fastest-growing obesity rates. Even in Europe, obesity rates have nearly tripled since 1975.
Why are we fatter than ever?
At a basic level, weight gain — eventually leading to being overweight or to obesity — is determined by a balance of energy. The obesity crisis of the past decades is best explained as the result of a rapid mismatch between our evolved biology and drastically changed modern environments, particularly in terms of food availability and physical activity levels. This mismatch, combined with socioeconomic factors and insufficient policy responses, has led to a global epidemic that affects countries at all levels of economic development.
Evolutionary perspective
In ancestral environments, humans were hunter-gatherers who relied on a diet consisting of wild plants, fruits, nuts, and animal protein. Food availability was unpredictable, leading to periods of feast and famine. This variability in food supply meant that humans evolved to store excess energy as fat during times of abundance to survive during times of scarcity.
The ability to store fat was an adaptive trait that provided a survival advantage. The "thrifty gene hypothesis" suggests that genes promoting efficient fat storage were selected for because they helped our ancestors survive periods of food scarcity.
Hunter-gatherers expended significant energy in daily activities, including hunting, foraging, and traveling long distances. Interestingly, research suggests that our ancestors did not necessarily expend more energy on physical activity compared to modern humans. Hadza foragers, for example, had higher physical activity levels, but their total daily energy expenditure was similar to Westerners when controlling for body size. However, hunter-gatherer lifestyles involved more diverse and frequent physical movements coupled with a diet of completely unprocessed foods. The abrupt shift from an active outdoor lifestyle to a sedentary indoor one is a major factor in the prevalence of obesity and chronic diseases in modern society.
Modern environment and lifestyle
Simply put, today we are eating more and moving less.
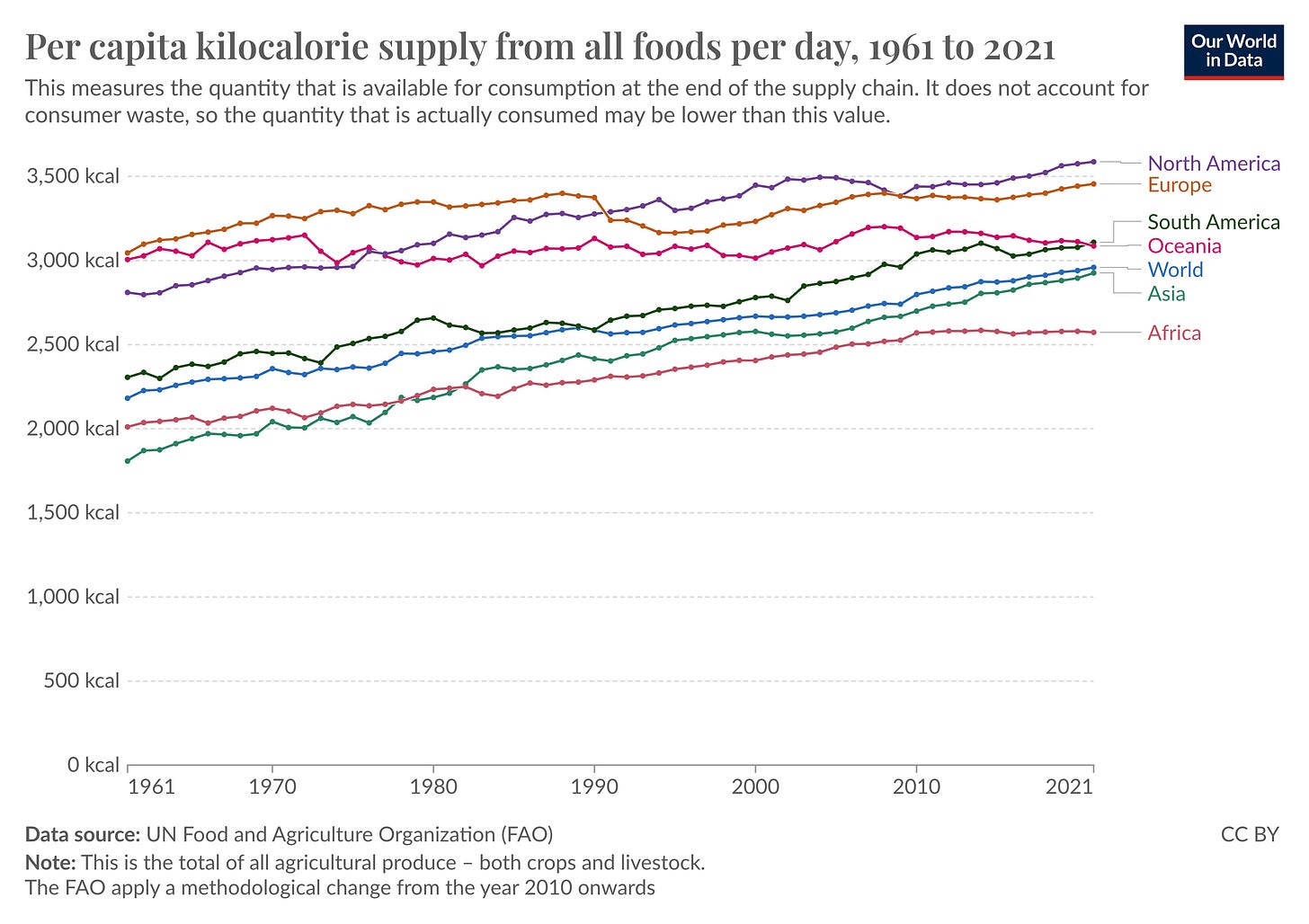
Our current global food environment is characterized by an abundance of high-calorie, nutrient-poor foods, often rich in sugar, fat, and refined carbohydrates. These foods are easily accessible and heavily marketed. The consumption of processed foods has increased, leading to a higher caloric intake than our ancestors experienced. In the 1960s, the global average supply of calories was around 2,200 kcal per person per day. By 2022, this had increased to 2960 kcal.
Modern lifestyles involve significantly less physical activity compared to our ancestors. Many people have sedentary jobs, use cars for transportation, and engage in fewer physical activities. The overall energy expenditure has decreased, which, when coupled with higher caloric intake, contributes to weight gain.
The human brain is wired to find pleasure in consuming high-calorie foods, a mechanism that once encouraged energy intake in times of plenty. However, this reward system can become overstimulated by the availability of hyper-palatable foods, leading to overeating. Our bodies are still wired to store excess calories efficiently and are driven to seek out calorie-dense foods, a beneficial trait in a food-scarce environment but maladaptive in today's calorie-rich world.
Socioeconomic and cultural factors
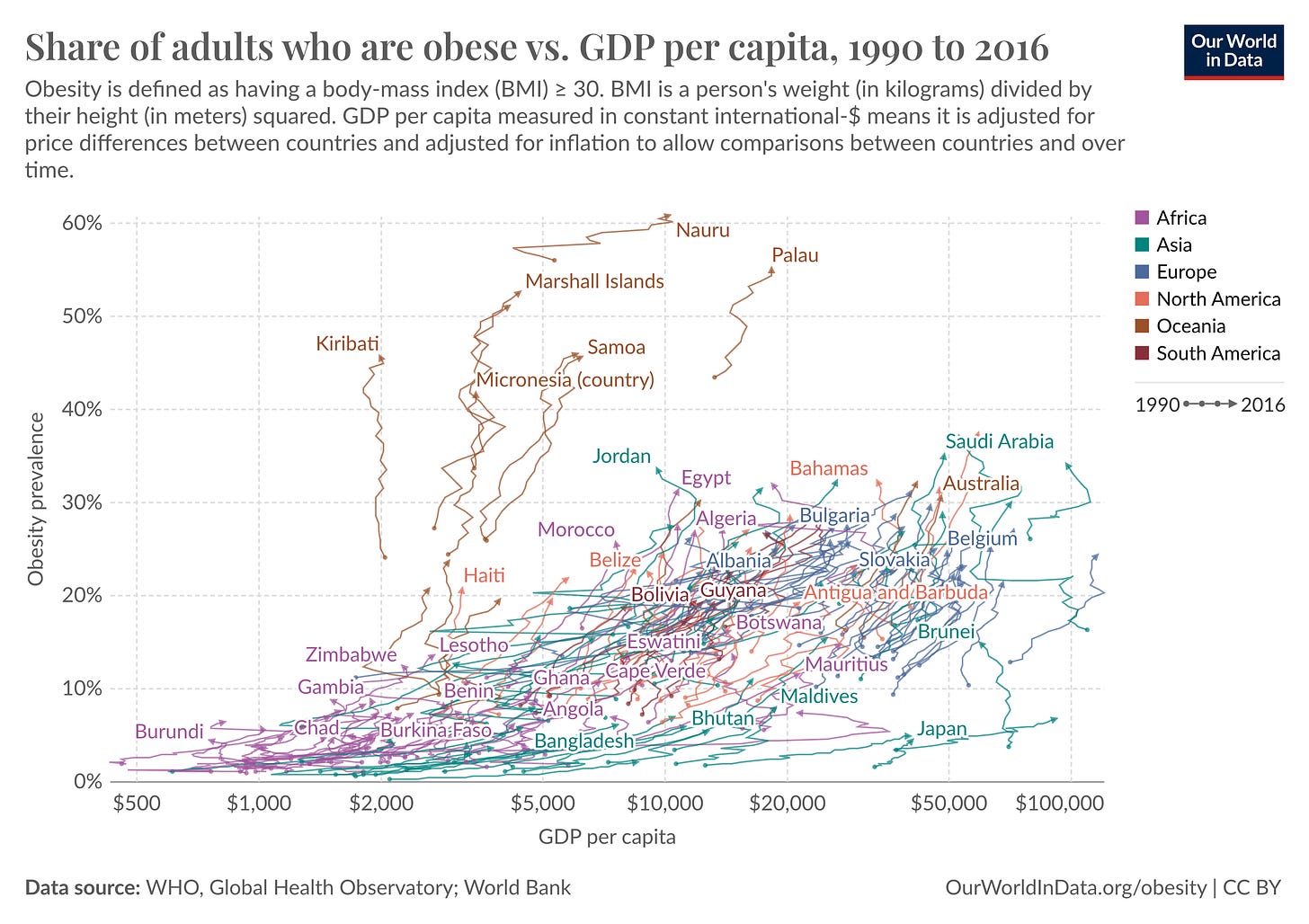
Obesity rates are increasing in almost every country, regardless of economic status. Both high-income and low- and middle-income countries are experiencing rising obesity rates. North America, Latin America, and the Caribbean currently exhibit some of the highest obesity rates, however, regions like sub-Saharan Africa and parts of Asia are also seeing rapid increases in obesity rates due to economic growth and urbanization. In countries like India and China, the prevalence of obesity in cities is three to four times the rate in rural areas, reflecting higher incomes in urban areas and therefore higher levels of nutrition and food consumption, often coupled with less active labor.
It is a common misconception that overweight and obesity are primarily problems in the United States. In reality, the obesity epidemic is a global issue affecting countries around the world, including those traditionally considered 'thin,' such as many European nations. For instance, in Italy, while only 17.8% of the population is classified as obese, more than 50% are currently overweight. Across Europe as a whole, approximately 53% of the adult population is overweight or obese. No member state in the WHO European Region is on track to reach the Sustainable Development Goal target of halting the rise in obesity by 2025.
What about genes?
Genetics can influence an individual's susceptibility to weight gain and obesity. Some people may be genetically predisposed to gain weight more easily or have difficulty losing weight. Studies suggest that genetics account for 40-70% of the variation in body weight among individuals. This means that people can inherit a predisposition to obesity, which can influence factors like appetite regulation, metabolism, fat storage, and how the body burns calories.
However, research also shows that environmental factors may be more impactful than genetic factors. For instance, someone with a genetic predisposition to obesity may not become obese if they have a healthy diet and active lifestyle. Conversely, someone with a lower genetic risk may still develop obesity if exposed to an obesogenic environment.
Irrespective of an individual’s predisposition, at a macro level, genetic changes are unlikely to account for the rapid rise in global obesity. The gene pool, which represents the distribution of different genes within a population, tends to remain consistent over many generations. It takes a considerable amount of time for new genetic mutations or variations to become widespread.
If our genes have largely remained unchanged, then what has altered in the past 40 years to cause increased obesity rates? The answer lies in our environment—the physical, social, and economic factors that shape our eating habits and activity levels.
Why is it so hard to lose weight?
While weight loss is possible, maintaining weight loss is notoriously challenging, with studies indicating that 80-85% of individuals who lose a significant amount of weight regain it within a few years.
This difficulty is rooted in evolutionary biology, where our bodies are programmed to resist weight loss to survive periods of famine. As I mentioned in the beginning, the "thrifty gene hypothesis" suggests that genes promoting efficient fat storage were positively selected because they provided a survival advantage during frequent famines. These genes, however, have become maladaptive in modern environments where high-calorie foods are readily available.
The set point theory further complicates this by suggesting that each individual has a biologically predetermined weight range that their body strives to maintain, regulated by complex feedback mechanisms involving hormones like leptin (satiety) and ghrelin (hunger). When a person loses weight, their body responds by decreasing metabolic rate and increasing hunger signals to restore the lost weight, making sustained weight loss challenging. This theory explains why many people experience weight loss plateaus and often regain weight after dieting. The set point is thought to be an evolutionary adaptation to protect against starvation, ensuring that the body holds onto energy reserves during times of caloric deficit. However, this mechanism, which was beneficial in environments with food scarcity, is less useful in today's world of constant food availability. In short, our bodies fight more against weight loss than weight gain.
One perspective that I find particularly interesting is that of Stephan Guyenet in his book, The Hungry Brain. His model explains the inefficacy of traditional weight loss strategies by highlighting the fundamental mismatch between our brain's evolutionary wiring and the modern food environment. Guyenet argues that our brains are hardwired to seek out calorie-dense, highly palatable foods, which were scarce in our ancestral environment but are now ubiquitous. This leads to overeating and weight gain because our brain's reward systems are easily hijacked by these foods, making it difficult to resist them. Traditional weight loss strategies, which often rely on conscious decision-making and willpower, fail to address these deep-seated neural circuits that drive eating behavior. His insights suggest that more effective weight loss strategies need to consider the neurobiological factors that influence eating behavior and develop interventions that can modulate these brain circuits.
Current obesity treatments
A note on how we measure obesity
Obesity is primarily measured using Body Mass Index (BMI), which is calculated by dividing a person's weight in kilograms by their height in meters squared. The World Health Organization (WHO) defines overweight as a BMI of 25 or higher, and obesity as a BMI of 30 or higher. While BMI is widely used due to its simplicity and low cost, it has limitations as it doesn't account for differences in body composition, muscle mass, or fat distribution across diverse populations. To complement BMI, some global health surveys also use waist circumference measurements to assess abdominal obesity.
Current treatments
To date, the most common and historically successful approaches to obesity treatment have included:
Lifestyle modifications:
Dietary changes: reducing calorie intake, increasing consumption of whole foods while limiting processed foods.
Increased physical activity: regular exercise and increased daily movement.
Behavior changes: modifying eating habits, addressing emotional eating, and developing healthier coping mechanisms.
Medications:
FDA-approved weight-loss medications such as orlistat, phentermine-topiramate, and liraglutide, used in conjunction with lifestyle changes.
Surgical interventions (for severe obesity):
Bariatric surgery procedures like gastric bypass, sleeve gastrectomy, and adjustable gastric banding.
Bariatric surgery has been the most effective in terms of significant and sustained weight loss. Patients typically lose 30-50% of their excess weight within 6 months post-surgery and up to 77% within 12 months. On average, they maintain 50% of their excess weight loss 5 years after surgery. This efficacy is due to the physiological changes induced by surgery, which alter the digestive system and reduce calorie absorption. However, surgery is invasive, carries risks of complications, and requires lifelong dietary changes and medical follow-up.
In contrast, lifestyle modifications and medications are less invasive but often result in more modest weight loss and are harder to maintain long-term. Lifestyle changes alone can lead to a 5-10% weight loss, which is often regained without ongoing support. Medications can enhance weight loss by an additional 3-12% when combined with lifestyle changes, but weight is often regained once the medication is stopped.
The National Institutes of Health (NIH) states that it is nearly impossible for people with class III obesity (BMI ≥ 40) to sustain weight loss through diet and exercise alone.
GLP-1 drugs
GLP-1 receptor agonists (GLP-1 RAs), the latest and most promising class of weight loss drugs, are unique in their dual ability to effectively manage both type 2 diabetes and obesity. They work by controlling blood glucose levels, suppressing appetite, and reducing food intake. GLP-1s have shown remarkable efficacy, with newer formulations like semaglutide resulting in an average weight loss of 15-17%. This represents a significant breakthrough in obesity management, potentially approaching the weight loss achieved by bariatric surgery in a non-invasive form. The effectiveness of GLP-1 drugs is challenging obesity stigma and shifting perceptions towards viewing it as a treatable medical condition.
The market for GLP-1 drugs is expected to exceed $100 billion by 2030. Ongoing research is exploring combination therapies (such as tirzepatide, a dual GLP-1/GIP receptor agonist), oral formulations to improve convenience and adherence, and potential applications in treating other conditions like cardiovascular disease, heart failure, and liver disorders.
Like many other medications, the effects of GLP-1 receptor agonists on weight loss are typically not sustained once treatment is discontinued. This phenomenon is not unique to GLP-1 drugs but is common across various medications that address chronic conditions. When patients stop taking GLP-1s, they are likely to regain weight, similar to how discontinuing statins leads to a rebound in lipid levels. This occurs because GLP-1s work by suppressing appetite, slowing gastric emptying, and influencing metabolic processes while the medication is active in the body. Once the drug is no longer present, these effects cease, and the body tends to return to its previous state. Obesity treatment with GLP-1 medications is generally considered a long-term or indefinite therapy, rather than a short-term solution, to maintain the achieved weight loss.
For people already living with obesity, urgent care and access to treatment is the only real solution. Despite current limitations like high costs and supply constraints, the efficacy and multiple health benefits of GLP-1 drugs make them the most promising obesity treatment to date.
In the long run, however, prevention is the winning strategy because once you become overweight or obese, it becomes so much harder to lose weight.
TL;DR
Nearly 43% of adults and 16% of children worldwide are overweight, with over 1 billion people classified as obese.
Obesity among adults has more than doubled since 1990, and among children and adolescents, it has quadrupled.
Obesity significantly contributes to nearly all leading causes of death and is projected to have an economic impact of $4.32 trillion annually by 2035, approximately 3% of global GDP.
Economic growth, urbanization, and lifestyle changes have led to increased obesity rates across various regions, including sub-Saharan Africa and Asia.
Human bodies evolved to store fat as a survival mechanism during times of food scarcity. This genetic predisposition is now maladaptive in an environment with abundant food and low physical activity.
The "thrifty gene hypothesis" and the set-point theory explain why it is difficult to maintain weight loss. The body tends to resist weight loss by slowing metabolism and increasing hunger signals.
GLP-1 receptor agonists are the most promising treatment for weight management, offering 15-17% average weight loss. However, weight tends to return after discontinuation, indicating the need for ongoing treatment.
While treating existing obesity is essential, prevention remains crucial. Preventing obesity, particularly in children, could be a more effective long-term strategy as losing weight becomes increasingly difficult once overweight or obese.
In next week’s post, I will cover everything we know about obesity prevention and explain why I believe that one of the most powerful strategies we can employ is to focus on preventing child obesity.